ECG MYOCARDIAL INFARCTION
Introduction to ECG Analysis
Electrocardiogram (ECG) analysis plays a pivotal role in the diagnosis and monitoring of various heart conditions. Understanding the significance of ECG in healthcare settings is essential for healthcare professionals, including doctors, paramedical staff, and individuals with a vested interest in heart health.
Importance of ECG in Diagnosing Heart Conditions
ECG is a non-invasive test that records the electrical activity of the heart and provides valuable insights into its functioning. By analyzing the ECG waveform, healthcare providers can identify abnormalities in the heart’s rhythm and structure, making it a crucial tool for diagnosing a wide range of cardiac issues.
The ability of ECG to detect irregularities in the heart’s electrical impulses enables healthcare professionals to promptly diagnose conditions such as arrhythmias, conduction disorders, and ischemic heart disease. Additionally, ECG monitoring is instrumental in assessing the efficacy of cardiac medications and interventions, aiding in the management of heart conditions.
To deepen your understanding of ECG analysis and its interpretation, you can explore our article on ecg interpretation for detailed insights into reading and deciphering ECG tracings.
Role of ECG in Detecting Myocardial Infarction
One of the critical applications of ECG is in the early detection of myocardial infarction, commonly known as a heart attack. Myocardial infarction occurs when blood flow to a part of the heart is blocked, leading to tissue damage and potential complications. ECG plays a pivotal role in promptly identifying the characteristic changes associated with myocardial infarction.
By examining specific ECG patterns such as ST-segment elevation, T-wave inversion, and Q-waves, healthcare providers can swiftly diagnose myocardial infarction and initiate appropriate interventions. Understanding the nuances of ECG changes in myocardial infarction is vital for optimizing patient outcomes and reducing the risk of complications.
For a comprehensive overview of ecg lead placement and other practical aspects of ECG analysis, refer to our article on ecg lead placement, which delves into the technical aspects of acquiring high-quality ECG tracings.
Understanding Myocardial Infarction
Myocardial infarction, commonly known as a heart attack, is a serious medical condition that occurs when there is a lack of blood flow to the heart muscle, leading to damage or death of heart tissue. Understanding the basics of myocardial infarction, including its definition, causes, and risk factors, is crucial for early detection and effective treatment.
What is Myocardial Infarction?
Myocardial infarction is a critical condition characterized by the sudden blockage of blood flow to a part of the heart muscle. This blockage is often caused by the formation of a blood clot in one of the coronary arteries, which are responsible for supplying oxygen-rich blood to the heart. Without an adequate blood supply, the affected area of the heart muscle begins to die, leading to chest pain or discomfort, known as angina, and potentially serious heart complications.
Causes and Risk Factors
Several factors can contribute to the development of myocardial infarction, including:
- Atherosclerosis: The buildup of plaque in the arteries, narrowing the blood vessels and reducing blood flow to the heart.
- Hypertension: High blood pressure increases the workload on the heart and can damage the blood vessels over time.
- Diabetes: Individuals with diabetes are at higher risk of developing cardiovascular diseases, including myocardial infarction.
- Smoking: Tobacco use can damage the blood vessels and promote the formation of blood clots, increasing the risk of heart attacks.
- Family History: A family history of heart disease can predispose individuals to a higher risk of myocardial infarction.
- Obesity: Excess weight and lack of physical activity can contribute to the development of conditions like atherosclerosis and hypertension, increasing the risk of heart attacks.
Understanding the causes and risk factors associated with myocardial infarction is essential for preventative measures and early intervention. By recognizing the symptoms and addressing the underlying risk factors, individuals can reduce their chances of experiencing a heart attack and improve their overall heart health. For more information on interpreting ECG findings related to myocardial infarction, visit our article on ECG interpretation.
In the next sections, we will explore the ECG changes observed in myocardial infarction and delve into the diagnostic criteria used to identify and classify different types of heart attacks.
ECG Changes in Myocardial Infarction
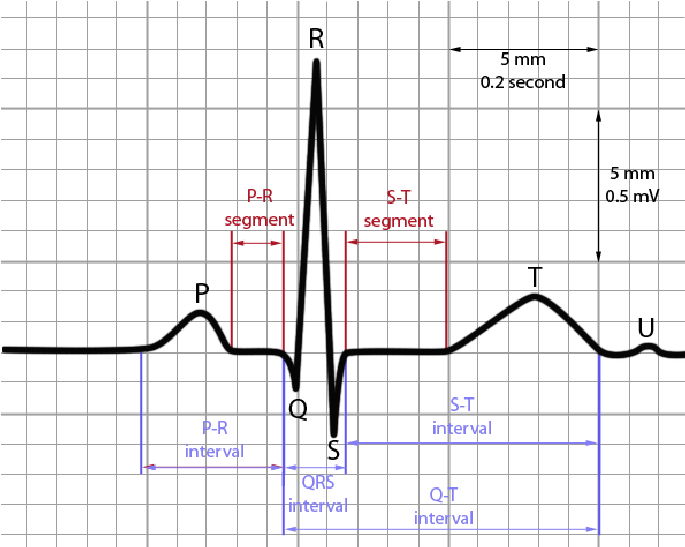
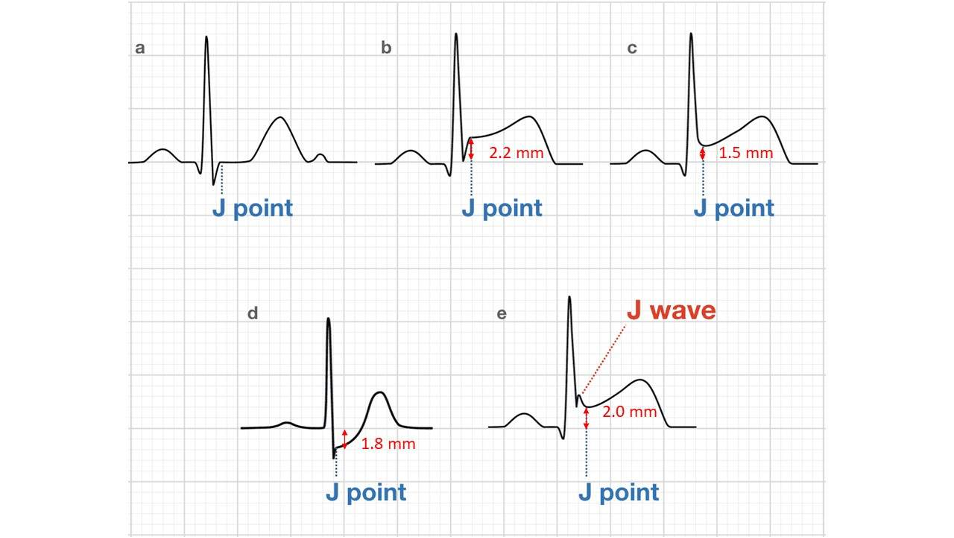
Within the realm of ECG analysis, specific changes can indicate the presence of myocardial infarction (MI). Understanding these ECG alterations is crucial for early detection and appropriate intervention. The key changes observed in myocardial infarction ECGs include ST-segment elevation, T-wave inversion, and Q-waves.
ST-Segment Elevation
ST-segment elevation is a hallmark feature of acute myocardial infarction on an ECG. It signifies transmural ischemia, where the full thickness of the heart wall is affected. This elevation is typically seen in the leads facing the area of infarction and is an urgent indicator for potential intervention. Below are the common leads associated with ST-segment elevation in specific areas of the heart:
| Area of Heart | Leads Showing ST-Segment Elevation |
|---|---|
| Anterior Wall | V1-V4 |
| Inferior Wall | II, III, aVF |
| Lateral Wall | I, aVL, V5-V6 |
T-Wave Inversion
In the context of myocardial infarction, T-wave inversion often follows ST-segment elevation or can occur in isolation. It is a common finding in the recovery phase of an MI, indicating repolarization abnormalities. T-wave inversion may persist beyond the acute phase, serving as a marker of myocardial injury. The presence of T-wave inversion in specific leads can provide valuable insights into the affected region of the heart.
| Area of Heart | Leads Showing T-Wave Inversion |
|---|---|
| Anterior Wall | V1-V4 |
| Inferior Wall | II, III, aVF |
| Lateral Wall | I, aVL, V5-V6 |
Q-Waves
Q-waves on an ECG are indicative of previous myocardial infarction and represent scar tissue formation in the myocardium. These pathological Q-waves are observed after the acute phase of MI and persist over time. The presence of Q-waves can give clinicians important information about the location and extent of prior myocardial damage.
| Location of Q-Waves | Implications |
|---|---|
| Anterior Q-Waves | Anterior wall MI |
| Inferior Q-Waves | Inferior wall MI |
| Lateral Q-Waves | Lateral wall MI |
Understanding the ECG changes associated with myocardial infarction, including ST-segment elevation, T-wave inversion, and Q-waves, is essential for timely diagnosis and management. Recognizing these patterns in ECG tracings can guide healthcare professionals in delivering appropriate care to patients presenting with suspected myocardial infarction. For more insights on ECG interpretation and analysis, explore our article on ecg interpretation.
Diagnostic Criteria for Myocardial Infarction
In the realm of Electrocardiogram (ECG) analysis, understanding the diagnostic criteria for myocardial infarction is fundamental for accurate interpretation and timely intervention. This section delves into the definitions and types of myocardial infarction, shedding light on the key aspects in diagnosing this critical cardiac event.
Definition of Acute Myocardial Infarction
Acute myocardial infarction (MI), commonly known as a heart attack, occurs when there is a sudden blockage of blood supply to a part of the heart muscle, leading to tissue damage. This disruption in blood flow is often caused by a blood clot in one of the coronary arteries, resulting in oxygen deprivation to the affected area.
One of the hallmark features of acute MI is the presence of specific ECG changes that signify myocardial injury. These changes manifest as deviations in the ST segment, T wave, and sometimes the development of pathological Q waves. Recognizing these patterns on the ECG tracing is essential for promptly diagnosing and managing myocardial infarction.
Types of Myocardial Infarction
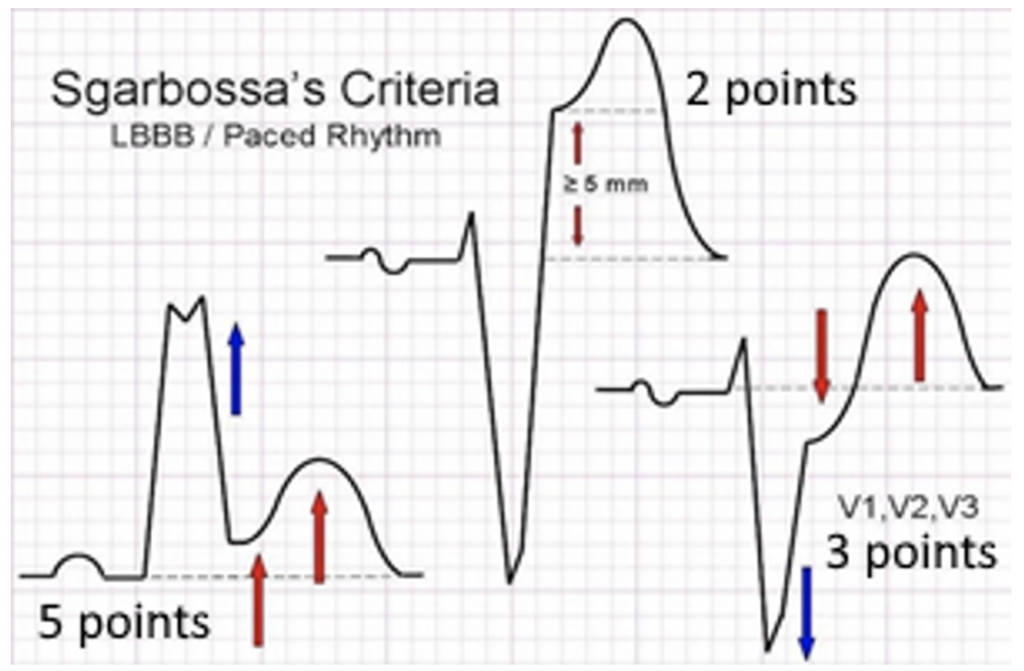
Myocardial infarction can be classified into several types based on the characteristics of the cardiac event and the underlying mechanism of injury. The two primary types of myocardial infarctions are ST-segment elevation myocardial infarction (STEMI) and non-ST-segment elevation myocardial infarction (NSTEMI).
- ST-Segment Elevation Myocardial Infarction (STEMI): STEMI is characterized by significant ST-segment elevation on the ECG tracing, indicative of complete occlusion of a coronary artery. This type of myocardial infarction typically requires urgent reperfusion therapy, such as thrombolytic treatment or primary percutaneous coronary intervention (PCI), to restore blood flow to the affected myocardium.
- Non-ST-Segment Elevation Myocardial Infarction (NSTEMI): NSTEMI, on the other hand, presents with ECG changes such as ST depression or T-wave inversion, signaling partial blockage or transient ischemia in a coronary artery. The management of NSTEMI involves a comprehensive assessment of the patient’s risk factors and may include strategies for medical stabilization and risk stratification.
By understanding the definitive criteria and differentiating between the types of myocardial infarction, healthcare professionals can make informed decisions regarding the diagnosis, treatment, and prognosis of patients presenting with acute cardiac symptoms. Continuous education and training in ECG analysis are paramount for enhancing clinical skills and ensuring accurate interpretation in critical situations. For more insights on ECG interpretation and heart investigations, explore our article on ECG interpretation.
Interpretation and Analysis
When it comes to interpreting an Electrocardiogram (ECG) in the context of myocardial infarction, healthcare professionals need to be adept at differentiating between various types of infarctions and identifying the location and severity of the damage.
Differentiating Between Types of Infarctions
Understanding the different types of myocardial infarctions is crucial for accurate diagnosis and treatment planning. The main types include:
| Type of Infarction | Description |
|---|---|
| STEMI (ST-Segment Elevation Myocardial Infarction) | Characterized by significant ST-segment elevation on the ECG. This type of infarction generally indicates a complete blockage of a coronary artery, requiring prompt intervention to restore blood flow. |
| NSTEMI (Non-ST-Segment Elevation Myocardial Infarction) | In NSTEMI, there may be subtle ECG changes such as ST-segment depression or T-wave inversion. This type of infarction is associated with partial blockages in the coronary arteries and necessitates close monitoring and potential interventions. |
Accurately differentiating between these types of infarctions is essential for providing the appropriate medical management and interventions tailored to each patient’s condition.
Identifying Location and Severity
In addition to distinguishing between types of infarctions, ECG analysis plays a vital role in identifying the location and severity of myocardial damage. Specific ECG changes can provide valuable insights into the affected area of the heart:
| ECG Finding | Implications |
|---|---|
| Anterior Infarction | ST-segment elevation in leads V1 to V4, indicating damage to the front of the heart. This type of infarction is associated with a higher risk of complications. |
| Inferior Infarction | ST-segment elevation in leads II, III, and aVF, suggesting damage to the inferior part of the heart. Patients with inferior infarctions may require specific treatment strategies. |
| Lateral Infarction | ST-segment elevation in leads I, aVL, V5, and V6, indicating damage to the lateral wall of the heart. Lateral infarctions can have significant implications for cardiac function. |
By accurately identifying the location and severity of myocardial infarction based on ECG findings, healthcare providers can make informed decisions regarding treatment options, risk stratification, and ongoing management for patients presenting with cardiac symptoms.
For further guidance on ECG interpretation, including lead placement and heart rate calculation, refer to our articles on ecg lead placement and ecg heart rate calculation. Stay updated and continue to enhance your skills in ECG analysis to ensure optimal patient care and outcomes.
Early Detection Methods
Early detection of myocardial infarction is crucial in providing timely and effective medical intervention. Understanding the importance of early detection and knowing the necessary precautions and immediate actions can significantly impact patient outcomes.
Importance of Early Detection
Early detection of myocardial infarction can mean the difference between life and death for patients. The quicker a heart attack is identified, the sooner appropriate measures can be taken to minimize damage to the heart muscle and improve the chances of recovery. This underscores the vital role that electrocardiography (ECG) plays in the early detection of myocardial infarction.
By recognizing the characteristic ECG changes associated with myocardial infarction, healthcare providers can promptly initiate the appropriate treatment protocols, such as administering thrombolytic therapy or arranging for urgent invasive procedures like angioplasty. This swift response can help mitigate the impact of the heart attack and prevent complications.
Precautions and Immediate Actions
For healthcare professionals tasked with interpreting ECGs, it is essential to be vigilant and proactive in identifying signs of myocardial infarction. Any suspicion of myocardial infarction based on ECG findings should trigger an immediate response to ensure the best possible patient outcomes.
Immediate actions upon suspecting myocardial infarction include:
- Notifying the Medical Team: Informing the attending physician or cardiologist of the ECG findings indicating myocardial infarction.
- Preparing for Interventions: Assembling the necessary equipment and personnel for potential emergent interventions.
- Monitoring the Patient: Continuously monitoring the patient’s vital signs and symptoms for any signs of deterioration.
- Administering Medications: Initiating appropriate medications to alleviate symptoms and stabilize the patient.
- Preparing for Transfer: Arranging for the transfer of the patient to a specialized cardiac care unit for further management.
Prompt action based on ECG findings is critical in the early management of myocardial infarction. Healthcare providers must be well-versed in recognizing ECG changes indicative of myocardial infarction and be prepared to act swiftly to ensure the best possible outcomes for their patients. For more insights on ECG interpretation and diagnostic criteria, refer to our article on ECG interpretation.
Case Studies and Examples
When it comes to understanding myocardial infarction, examining real-life case studies and ECG tracings can provide invaluable insights for healthcare professionals. By analyzing these cases, medical professionals can enhance their diagnostic skills and improve patient outcomes.
ECG Tracings of Myocardial Infarction Cases
Studying ECG tracings from actual myocardial infarction cases allows practitioners to observe the characteristic changes that occur during an acute event. These tracings often exhibit specific patterns, such as ST-segment elevation, T-wave inversion, and Q-waves, which are indicative of myocardial damage. Understanding and identifying these patterns are essential for accurate diagnosis and timely intervention.
Below is a simplified representation of ECG findings commonly associated with myocardial infarction:
| ECG Feature | Description |
|---|---|
| ST-Segment Elevation | Indicates acute myocardial injury and is a hallmark of ST-segment elevation myocardial infarction (STEMI). |
| T-Wave Inversion | Can signify myocardial ischemia and is often seen in the subacute phase of myocardial infarction. |
| Q-Waves | Represent irreversible myocardial necrosis and are typically observed in the chronic phase of myocardial infarction. |
Analysis and Discussion on Case Studies
Analyzing ECG tracings from myocardial infarction cases involves a comprehensive review of the presented clinical scenarios. By examining the patient’s medical history, symptoms, risk factors, and ECG findings, healthcare providers can piece together crucial information to formulate an accurate diagnosis and treatment plan.
Moreover, discussing these case studies with colleagues and experts in the field can offer different perspectives and insights into complex cardiac presentations. Through collaborative analysis and discussion, healthcare professionals can enhance their diagnostic acumen and broaden their understanding of myocardial infarction management.
Continuing education and exposure to diverse case studies are essential for staying abreast of the latest advancements in ECG analysis and myocardial infarction diagnosis. By actively engaging in case-based learning, healthcare professionals can refine their skills, refine diagnostic accuracy, and ultimately improve patient care outcomes.
Continuing Education in ECG Analysis
For healthcare professionals and individuals involved in interpreting electrocardiograms (ECGs), ongoing education in ECG analysis is essential to ensure accurate diagnoses and optimal patient care. Continuous learning not only enhances expertise but also keeps practitioners updated with the latest advancements in ECG interpretation techniques and guidelines.
Further Resources for ECG Learning
To deepen your knowledge and sharpen your skills in ECG analysis, there are various resources available that cater to different learning preferences. These resources can provide valuable insights, case studies, and practical tips for mastering ECG interpretation. Some recommended sources for further ECG learning include:
| Resource Type | Description |
|---|---|
| Online Courses | Interactive ECG courses with quizzes and case studies. |
| Textbooks | Comprehensive guides on ECG interpretation and myocardial infarction diagnosis. |
| ECG Workshops | Hands-on workshops for practical experience in ECG analysis. |
| Medical Journals | Research articles and studies on ECG changes in myocardial infarction cases. |
By exploring these resources, healthcare professionals can enhance their proficiency in ECG analysis and stay informed about the latest developments in cardiac care.
Importance of Regular Training and Updates
Regular training and updates in ECG analysis are crucial for maintaining competence and staying abreast of advancements in cardiovascular medicine. Continuous education not only reinforces existing knowledge but also introduces new concepts and techniques that can improve diagnostic accuracy and patient outcomes.
In the fast-evolving field of cardiology, staying current with guidelines, diagnostic criteria, and emerging technologies is essential. Training programs and refresher courses can help healthcare professionals refine their ECG interpretation skills, recognize subtle changes in ECG tracings, and identify potential indicators of myocardial infarction early on.
Moreover, ongoing education fosters a culture of lifelong learning and promotes excellence in patient care. By dedicating time to professional development and keeping pace with the latest trends in ECG analysis, healthcare providers can enhance their diagnostic abilities, contribute to better patient outcomes, and uphold the highest standards of cardiac care.
For healthcare practitioners and individuals involved in ECG analysis, a commitment to continuous learning is paramount in ensuring proficiency, accuracy, and innovation in the detection and management of myocardial infarction cases.