7 Key Indications for a Permanent Pacemaker: What You Need to Know
Permanent Pacemaker Indications: Imagine your heart as a symphony orchestra. Each beat, a perfect note played in rhythm, keeps the music of life flowing. But what happens when the conductor falters? A permanent pacemaker steps in as the maestro, ensuring the heart maintains its perfect tempo. This tiny device can be a lifesaver for many people facing heart rhythm issues. Let’s delve into what a pacemaker is, why it’s essential, and the seven critical reasons someone might need this life-enhancing technology.
Also Read: Revolutionize Your Health: 6 Ways Medical Robotics Are Changing the Game
Understanding Pacemakers
What is a Pacemaker?
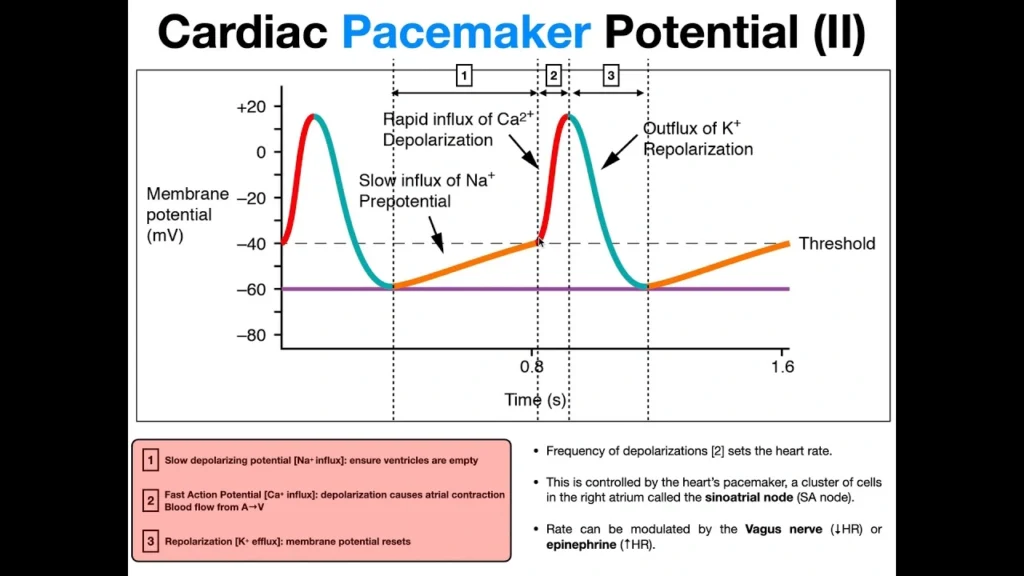
A pacemaker is a small, battery-operated device implanted in the chest to help manage irregular heartbeats. It sends electrical impulses to prompt the heart to beat at a normal rate.
How Does a Pacemaker Work?
The pacemaker consists of a generator, which houses the battery and the control center, and leads (or electrodes), which transmit electrical signals to the heart. When the pacemaker detects an abnormal heart rhythm, it sends signals to correct it.
Types of Pacemakers
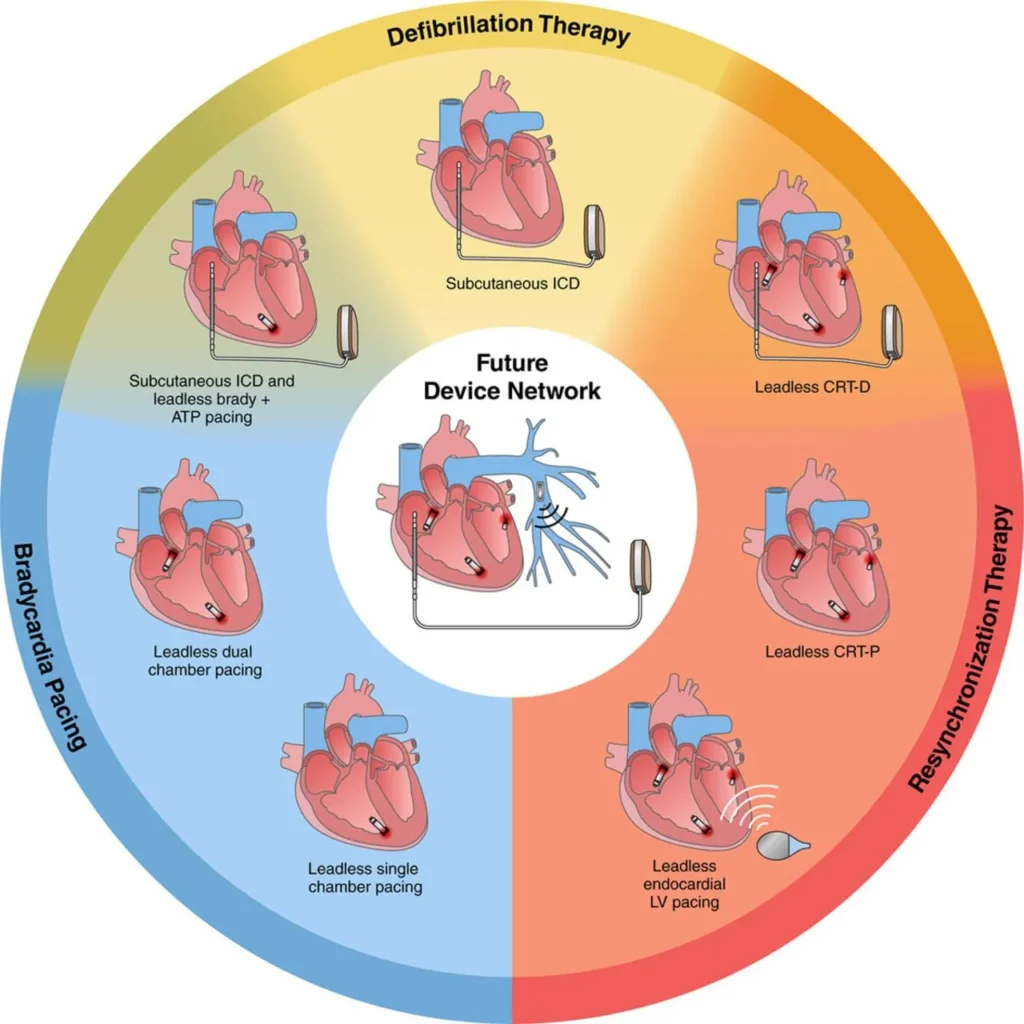
There are several types of pacemakers, including:
- Single-chamber pacemakers: Connect to one chamber of the heart.
- Dual-chamber pacemakers: Connect to two chambers.
- Biventricular pacemakers: are used for cardiac resynchronization therapy, connecting to both ventricles.
Permanent Pacemaker Indications:
When is a Pacemaker Needed?
Pacemakers are critical for individuals with certain heart conditions. The following sections outline the seven primary reasons for needing a permanent pacemaker.
Critical Reason 1: Bradycardia
Definition and Symptoms
Bradycardia is a condition characterized by an abnormally slow heart rate, typically fewer than 60 beats per minute. Symptoms include fatigue, dizziness, and fainting spells.
How a Pacemaker Helps
A pacemaker monitors the heart rate and sends electrical signals to increase the heart rate when it drops too low, thereby alleviating symptoms and improving the patient’s quality of life.
Critical Reason 2: Heart Block
Types of Heart Block
A heart block occurs when the electrical signals that control the heartbeat are partially or completely blocked. There are three degrees:
- First-degree: Partial block, minor symptoms.
- Second-degree: More severe block, occasional missed beats.
- Third-degree: Complete block, serious symptoms requiring immediate intervention.
Pacemaker’s Role in Treatment
A pacemaker can bypass the blockage, restoring normal heart rhythm and preventing complications associated with insufficient blood flow.
Critical Reason 3: Atrial Fibrillation
Understanding Atrial Fibrillation
Atrial fibrillation (AFib) is an irregular, often rapid heart rate that can lead to blood clots, stroke, and other heart-related complications.

Pacemaker as a Treatment Option
In cases where medication and other treatments fail, a pacemaker can help manage the heart rate, reducing the risk of complications and improving overall heart function.
Critical Reason 4: Heart Failure
How Heart Failure Affects Heart Rhythm
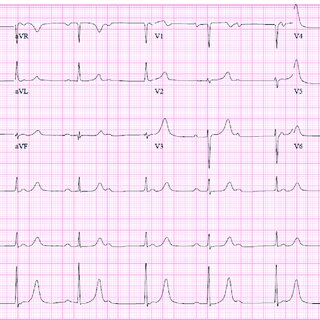
Heart failure occurs when the heart cannot pump enough blood to meet the body’s needs. This can cause arrhythmias, which worsen the condition.
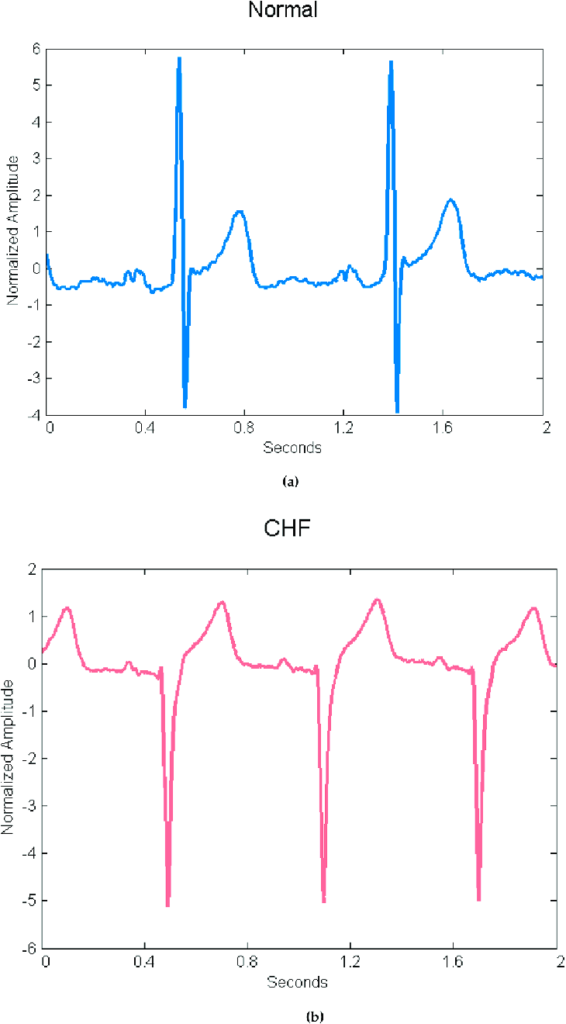
Benefits of a Pacemaker
A pacemaker, particularly a biventricular one, can synchronize the contractions of the heart’s ventricles, improving the efficiency of the heart’s pumping action and alleviating symptoms of heart failure.
Critical Reason 5: Syncope
What is Syncope?
Syncope is a sudden, temporary loss of consciousness, commonly known as fainting, often caused by a drop in heart rate or blood pressure.
Pacemaker’s Effectiveness in Preventing Fainting
For individuals experiencing recurrent syncope due to heart rhythm issues, a pacemaker can prevent these episodes by maintaining a steady heart rate, thereby reducing the risk of injury from fainting.
Critical Reason 6: Post-Heart Attack Complications
Impact of Heart Attack on Heart Rhythm
A heart attack can damage the heart muscle, leading to irregular heartbeats (arrhythmias) that can be life-threatening if not managed properly.
Role of Pacemaker in Recovery
A pacemaker can help stabilize the heart rhythm post-heart attack, aiding in the recovery process and preventing further cardiac events.
Critical Reason 7: Congenital Heart Conditions
Overview of Congenital Heart Defects
Congenital heart defects are structural problems with the heart present at birth, which can lead to abnormal heart rhythms.
Pacemaker Use in Congenital Cases
For some congenital heart conditions, a pacemaker is necessary to ensure a regular heart rhythm, improving the child’s growth, development, and overall health.
The Pacemaker Implantation Procedure
Pre-Procedure Preparations
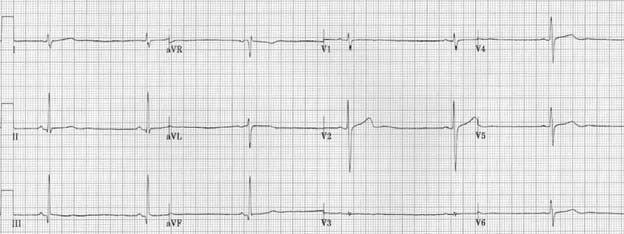
Before implantation, doctors perform various tests, including ECG, echocardiogram, and stress tests, to ensure the patient is a good candidate for a pacemaker.
The Implantation Process
The procedure typically takes a few hours and is performed under local anesthesia. The device is implanted just under the skin near the collarbone, and the leads are threaded through a vein to the heart.
Post-Procedure Care
After the procedure, patients usually stay in the hospital overnight for monitoring. Recovery involves avoiding strenuous activities for a few weeks and regular follow-up appointments to check the pacemaker’s function.
Living with a Pacemaker
Daily Life Adjustments
Most people can return to normal activities after recovery. However, they should avoid close proximity to strong electromagnetic fields, which can interfere with the pacemaker.
Long-Term Care and Monitoring
Regular check-ups are essential to ensure the pacemaker is functioning correctly. This includes remote monitoring and occasional adjustments by a healthcare professional.
Potential Complications and How to Avoid Them
Complications are rare but can include infection, lead displacement, or battery failure. Following the doctor’s advice and maintaining regular follow-ups can minimize these risks.
Advancements in Pacemaker Technology
Latest Innovations
Recent advancements include leadless pacemakers, which are smaller and have fewer complications, and MRI-compatible pacemakers that allow patients to undergo MRI scans safely.
Future Prospects
Future innovations may include rechargeable batteries, improved remote monitoring, and pacemakers that can adjust their settings automatically based on the patient’s activity level.
Conclusion
Pacemakers are a remarkable blend of medical technology and lifesaving intervention. For those facing severe heart rhythm issues, these tiny devices ensure that the heart beats correctly, providing a new lease on life. Understanding the critical reasons for needing a pacemaker helps demystify the process and underscores the profound impact this technology has on individuals’ health and well-being.
FAQs
Q: What is the lifespan of a pacemaker?
Most pacemakers last between 5 to 15 years, depending on usage and the type of device. Regular check-ups help monitor battery life.
Q: Can I live a normal life with a pacemaker?
Yes, most people with pacemakers lead normal, active lives with minimal restrictions.
Q: Are there any activities I should avoid with a pacemaker?
Avoid activities that involve strong magnetic or electrical fields. Heavy lifting and contact sports may also be restricted shortly after implantation.
Q: How often do I need to check my pacemaker?
Regular check-ups are typically scheduled every 3 to 6 months, but remote monitoring can provide continuous oversight.
Q: What are the signs that my pacemaker might need adjustment?
Signs include dizziness, fatigue, palpitations, or swelling at the implantation site. Contact your doctor if you experience any of these symptoms.
